Abstract
Introduction: The objective was to evaluate the mortality and the morbidity in neonates operated for persistent ductus arteriosus at Copenhagen University Hospital in the 10-year period from 1 January 1998 to 31 December 2007, and to compare the results with results reported in extant literature.
Material and methods: Patient data were collected by retrospective audit of medical charts. Infants with complex heart disease were excluded. The outcomes were mortality, necrotising enterocolitis (NEC), intraventricular haemorrhage (IVH), paresis of the recurrent laryngeal nerve and chylothorax. For statistical analyses, we used Fisher’s exact test and Mann-Whitney U test.
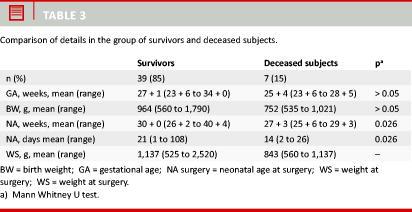
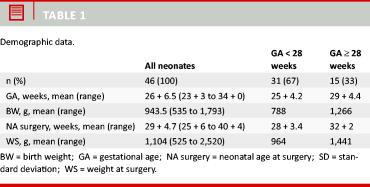
Results: We included 46 neonates among an initial 60 candidates. Gestational age was from 23 + 6 to 34 + 0 weeks (mean 26 + 6.5) and the birth weight ranged from 535 g to 1,793 g (mean 943.5 g). In 93% of cases, the left atrium diameter (LAD)/aorta diameter (Ao)-ratio measured by echocardiography was greater than or equal to 1.5, and medical closure had been attempted in 93% of the cases. After surgical ligation, there were three cases of paresis of the recurrent laryngeal nerve, two cases of chylothorax, eight cases of NEC, four cases of IVH and seven deaths (15.2%). The deaths occurred between three and 119 days postoperatively. Those who died were operated at an earlier age than the remaining patients (p < 0.05) and they tended to be of lower gestational age and to have a lower birth weight (p > 0.05) than those who survived.
Conclusion: The need for ligation of a patent arterial duct in preterm neonates is subject to considerable risk. Total mortality in this vulnerable group of patients was 15%. Although no obviously procedure-related deaths were observed, severe complications and postoperative morbidity occurred.
Abstract
Introduction: The objective was to evaluate the mortality and the morbidity in neonates operated for persistent ductus arteriosus at Copenhagen University Hospital in the 10-year period from 1 January 1998 to 31 December 2007, and to compare the results with results reported in extant literature.
Material and methods: Patient data were collected by retrospective audit of medical charts. Infants with complex heart disease were excluded. The outcomes were mortality, necrotising enterocolitis (NEC), intraventricular haemorrhage (IVH), paresis of the recurrent laryngeal nerve and chylothorax. For statistical analyses, we used Fisher’s exact test and Mann-Whitney U test.
Results: We included 46 neonates among an initial 60 candidates. Gestational age was from 23 + 6 to 34 + 0 weeks (mean 26 + 6.5) and the birth weight ranged from 535 g to 1,793 g (mean 943.5 g). In 93% of cases, the left atrium diameter (LAD)/aorta diameter (Ao)-ratio measured by echocardiography was greater than or equal to 1.5, and medical closure had been attempted in 93% of the cases. After surgical ligation, there were three cases of paresis of the recurrent laryngeal nerve, two cases of chylothorax, eight cases of NEC, four cases of IVH and seven deaths (15.2%). The deaths occurred between three and 119 days postoperatively. Those who died were operated at an earlier age than the remaining patients (p < 0.05) and they tended to be of lower gestational age and to have a lower birth weight (p > 0.05) than those who survived.
Conclusion: The need for ligation of a patent arterial duct in preterm neonates is subject to considerable risk. Total mortality in this vulnerable group of patients was 15%. Although no obviously procedure-related deaths were observed, severe complications and postoperative morbidity occurred.
Patent ductus arteriosus (PDA) is a frequent heart defect in premature babies. The incidence of PDA is inversely related to gestational age (GA) [1, 2]. In the foetus, the ductus arteriosus shunts blood from the pulmonary artery to the aorta, hereby bypassing the lungs. Func-tional closure of the ductus arteriosus normally occurs shortly after birth.
After birth a patent ductus arteriosus usually causes the blood to flow from the systemic circulation to the pulmonary circuit, i.e. a left-right shunt. This shunt results in an increased pulmonary perfusion and thus impairs pulmonary mechanics and/or decreases systemic perfusion. These haemodynamic changes may partly be responsible for the co-morbidity associated with PDA; such comorbidity includes hypotension, interventricular and pulmonary haemorrhage, necrotising enterocolitis (NEC) and chronic lung disease.
First-line treatment is fluid restriction, diuretics and ibuprofen or indomethacin [3]. Surgical PDA ligation is considered when first-line treatment has failed or is contraindicated. The aim of this study was to evaluate the mortality and the morbidity in neonates operated for persistent ductus arteriosus at Copenhagen University Hospital (CUH) in the 10-year period from 1 January 1998 to 31 December 2007 and to compare the results with the results in extant literature.
MATERIAL AND METHODS
Premature babies (GA < 37 + 0) who underwent PDA ligation and were born in the period from 1 January 1998 to 31 December 2007 were identified from the database maintained at the Department of Neonatology (GN) at the CUH.
The preoperative details collected included gestational age, birth weight, the left atrium diameter (LAD)/aorta diameter (Ao)-ratio of the PDA and the use of indomethacin or ibuprofen. Operative details included age and weight at ligation and the postoperative details recorded comprised outcome, age and cause of death. The presence of NEC, interventricular haemorrhage and paresis of the recurrent laryngeal nerve was also recorded.
The primary goal of the study was to evaluate mortality after surgical closure of PDA; therefore, the medical charts of any patients who died were further reviewed.
Univariate statistical analysis of the data was performed using Fisher's exact test on categorical comparisons of two populations and the Mann-Whitney U test on continuous data. All tests were two-sided and p-values below 0.05 were considered significant. 95% confidence intervals were used.
RESULTS
In the 10-year period, 60 premature babies were treated surgically for persistent ductus arteriosus at the GN. A total of 14 (23%) of the 60 neonates who underwent surgical ligation were excluded from this study, 12 (20%) because PDA was complicating another congenital heart disease, and two (3%) were excluded because their medical charts were missing. A total of 46 neonates were thus included in the study.
DEMOGRAPHIC DATA
PREOPERATIVE VARIABLES
All neonates had their PDA diagnosis confirmed by echocardiography performed by a paediatric cardiologist. The LAD/Ao-ratio was recorded in most cases (91%) and varied from 0.97 to 2.7 with an average of 1.9. In 93% of the cases, the ratio was above or equal to 1.5.
In most cases, the LAD/Ao-rate ratio used to support the operation indication of ‘‘haemodynamic instability’’, which was by far the most common indication for surgery. 71% of the patients were operated on such indication. Other indications mentioned were respiratory instability and echo findings, but they only constituted 15.4% and 9.6% of the indications, respectively. A clearly stated indication for surgery was found in almost all records (96%).
Medical closure of the PDA with ibuprofen or indomethacin was attempted prior to surgery in 39 out of 46 neonates (93%), which was in line with local guidelines [3]. In the seven neonates undergoing primary surgery, medical treatment was contraindicated because of NEC, IVH or pulmonary haemorrhage.
Prior to ductal ligation, the clinical course had been complicated in most patients: Thirty-two had been mechanically ventilated and 24 had been treated with vasopressors. NEC was diagnosed in 11 patients, three of whom had been treated surgically. Six patients were diagnosed with intraventricular haemorrhage (IVH). At the time of the operation, 39 (85%) were oxygen-dependent. The mean age at surgery among survivors was 21 days, which is significantly more than the 14 days of age in those who died (p = 0.026).
OPERATIVE AND POSTOPERATIVE MORBIDITY
There were no anaesthesia-related complications and no operative deaths. The incidence of NEC after ductal ligation was 8/46 (17%), whereof two also had NEC before surgery. In five patients, NEC was diagnosed within the first five days after surgery; the remaining three were diagnosed on days 12, 14 and 93 postoperatively.
Among the 11 patients who underwent PDA ligation within the first week of life, postoperative IVH was diagnosed in four patients (36%) (one grade two and three grade four cases). There were three (7%) cases of paresis of the recurrent laryngeal nerve and two cases (4%) of chylothorax.
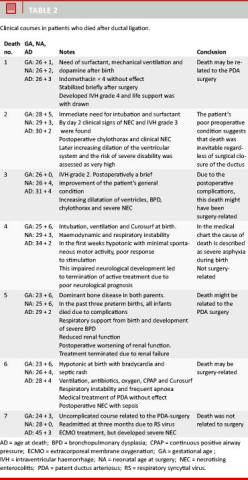
POSTOPERATIVE MORTALITY
Among the 46 neonates, there were seven deaths (15%), which occurred between three and 119 days after birth. Six patients (13%) died during the same admission and one (2%) during a subsequent admission (Table 2 and Table 3).
DISCUSSION
The mortality in the cohort was 4.3% at seven days postoperatively, 8.7% at 30 days, 13% at discharge and 15.2% overall. In comparison, the 30-day mortality in all planned and acute bypass surgery procedures performed at the CUH in 2001-2003 was 2.4% [4].
While there are clear local guidelines concerning the medical treatment of PDA, the decision to perform surgical ligation is based on an individual assessment of the clinical state of each infant. All patients in the non-surviving group were suffering from serious neonatal problems, which were typically circulatory instability, and the decision to operate was generally taken within the first weeks of life. In all cases, the decision to operate was supported by echocardiographic findings.
In the present study, the deaths therefore occurred primarily in children who were in poor condition prior to surgical ligation of the PDA. Nevertheless, only two deaths could with reasonably certainty be attributed to causes other than the surgery. Thus, the possibly surgery-related mortality was 10.9% (confidence interval (CI) 1.9%, 19.9%). On the other hand, no death in this study occurred in a stable patient who suddenly wor- sened after the PDA surgery.
The possibly surgery-related mortality of 10.9% is not to be interpreted as mortality which was likely caused by surgery, but rather as mortality in a group of very sick neonatal patients. The mortality rate thus cannot be used to change the indications for operation, but will rather serve as an explanation to parents as infants qualifying for operation belong to a very fragile group of premature infants.
Necrotising enterocolitis was frequent before as well as after surgery. This is not surprising in view of the low mean gestational age and as PDA is an independent risk factor for development of NEC [5].
We know that the the most of immature babies are at considerable risk of having a significant PDA [2] and that these babies more frequently do not respond to medical treatment and are also more prone to other complications. The surgical group therefore includes the most fragile and sick children [6, 7].
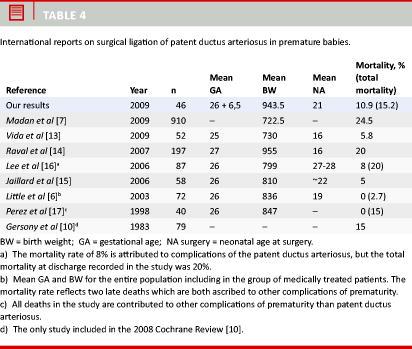
INTERNATIONAL EXPERIENCES
PDA treatment is subject to debate [8]. A Cochrane review from 2008 [9] identified one randomized con-trolled trial comparing outcomes of primary surgery with primary medical closure of PDA. This study [10] was performed in 1983 and evaluated neonates treated for PDA in the 1979-1982 period, i.e. before the use of antenatal glucocorticoids and postnatal surfactant became widespread; and the study concluded that the published data on the advantages/disadvantages of the treatments are insufficient for favouring one treatment over another.
A recent study [11] found that the risk of death without surgical ligation was four times higher for medical non-responders than for responders, and thus speaks for surgical ligation of PDA after attempted medical closure. Similarly, Kabra et al [12] found that among 426 preterms with PDA, the mortality rate for the group without surgical ligation was 22% versus 14% in the group with surgical closure (p < 0.05). Kabra et al, however, noted that the neonates with symptomatic PDA who were treated with surgical ligation had an increased risk of neurosensory impairment, bronchopulmonary dysplasia and retinopathy of prematurity. Two new studies from 2009 also make conflicting conclusions [7, 13] (Table 4).
There were not enough subjects in our study to analyse the effects of gestational age or birth weight on outcome, but further work on this would be useful since PDA is most prevalent in extremely premature babies. Raval et al [14] discussed this and concluded that a higher gestational age, higher birth weight and higher postnatal age at operation are associated with a lower risk of death, as, indeed, also indicated by the results from our study.
In summary, we feel that the mortality of up to 15.2% and the associated morbidity cannot be ignored, although the deaths might have been inevitable regardless of surgical closure of the PDA.
CONCLUSION
The need for ligation of a patent arterial duct in preterm neonates is subject to considerable risk. Total mortality in this vulnerable group of patients was 15%. Although there were no procedure-related deaths, severe complications and other postoperative morbidity occurred.
Correspondence: Cristel M. Sørensen, Åboulevard 14, 5. tv., 2200 København N, Denmark. E-mail: cristel.soerensen@gmail.com
Accepted: 25 April 2010
Conflicts of interest: None

REFERENCES
www.phsinfo.dk – ‘‘alle dokumenter’’ – ‘‘sorteret alfabetisk’’ – ‘‘Kardielle mislyde hos børn’’ (Jesper Reimers, Koncern Plan og Udvikling. 07-11-2006)" (16 April 2010).
Wyllie J. Treatment of patent ductus arteriosus. Sem Neonatol 2003;8:425-32.
www.rh-vejledninger.dk, search: »ductus arteriosus persistens«, result no. 1 (14 April 2010).
http://www.rigshospitalet.dk/menu/AFDELINGER/Hjertecentret/Thoraxkirurgisk+Klinik/Sygdom+og+behandling/ Statistik+om+bypass-kirurgi.htm (14 April 2010).
Dollberg S, Lusky A, Reichman B. Patent ductus arteriosus, indomethain and necrotizing enterocolitis in very low birth weight infants: A population-based study. J Pediatr Gastroenterol Nutr 2005;40:184-8.
Little DC, Pratt TC, Blalock SE et al. Patent ductus arteriosus in micropreemies and full-term infants: The relative merits of surgical ligation versus indomethacin treatment. J Ped Surg 2003;38:492-6.
Madan JC, Kendrick D, Hagadorn JI et al. Patent ductus arteriosus therapy: impact on neonatal and 18-month outcome. Pediatrics 2009;123:674-81.
Knigth DB. The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Semin Neonatol 2001;6:63-73.
Malviya M, Ohlsson A, Shah S. Surgical versus medical treatment with cyclooxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev 2008;(1):CD003951.
Gersony WM, Peckham GJ, Ellison RC et al. Effects of indomethacin in premature infants with patent ductus arteriosus: Results of a national collaborative study. J Pediatr 1983;102:895-906.
Brooks JM, Travadi JN, Doherty DA et al. Is surgical ligation of ductus arteriosus necessary? Arch Dis Child Fetal Neonatal Ed 2005;90:235-9.
Kabra N, Schmidt B, Roberts RS et al. Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the trial of indomethacin prophylaxis in preterms. J Pediatr 2007;150:229-34.
Vida VL, Salvatori S, Boccuzzo G et al. is there an optimal timing for surgical ligation of patent ductus arteriosus in preterm infants? Ann Thorac Surg 2009;87:1509-16.
Raval MV, Laughon MM, Bose CL et al. Patent ductus arteriosus ligation in premature infants: Who really benefits, and at what cost? J Ped Surg 2007;42:69-75.
Jaillard S, Larrue B, Rakza T et al. consequences of delayed surgical closure of patent ductus arteriosus in very premature infants. Ann Thorac Surg 2006;81:231-5R.
Lee L, Tillet A, Tulloh R et al. Outcome following patent ductus arteriosus ligation in premature infants: a retrospective cohort analysis. BMC Pediatrics 2006;6:15.
Perez CA, Bustorff-Silva JM, Villasenor E et al. surgical ligation of patent ductus arteriosus in very low birth weigth infants: Is it safe? Am Surg 1998;64:1007-9